I have a confession. If I had been diagnosed with celiac disease, I could have been a celiac snob. In fact, it’s highly likely I would have been a celiac snob.
Some gfe discussion posts address “prickly” topics. I usually have them in my head for months, sometimes years (as is the case for today’s post) and then I finally start writing them, working on them “here and there” long before they get published, sometimes delaying their publication because I just can’t get my words to feel right and/or I’m not sure I’m ready for the actual discussion that will ensue.
This post is such a post. I generally work on my discussion posts until they are nice and coherent with a smooth flow, and some do eventually come together fairly nicely, but, sadly, some never do. This one is one of the latter. I don’t consider it in final form and I don’t consider it polished and ready to go, but I feel that I just need to finally publish it. That’s especially true considering all the publicity in the last week or so on gluten sensitivity not being “real.”
So I have to go forward with this post, even though it’s unbelievably long. A topic like this one can’t be discussed in 500 words or less. I appreciate you taking the time to read my ramblings.
If you’ve seen the recent media hype on non-celiac gluten sensitivity, the naysayers have been having quite a field day in the media, haven’t they? I won’t talk too much about that and won’t even link to these ridiculous articles except to say that the study cited in these numerous poorly written and incendiary articles was a very small study (37 individuals) and the research is ongoing. The study being cited as proof that only celiac is “real” actually was published early last year. In my opinion, Mark Sisson of Mark’s Daily Apple has the best response to date on the study and all the articles. And by the way, have you ever noticed how small studies are disregarded when they don’t agree with others’ beliefs and agendas, but exalted when they do?
There’s much more that can be said on this topic, but experts like Dr. Alessio Fasano state emphatically that non-celiac gluten sensitivity does exist. If you’re not familiar with Dr. Fasano, he’s the chief of MassGeneral Hospital for Children’s Division of Pediatric Gastroenterology and Nutrition and director of the hospital’s Center for Celiac Research. He is one of the world’s foremost experts on celiac disease and gluten issues other than celiac, which he calls gluten-related disorders. We have him to thank for the landmark study in 2003 that established the incidence of celiac disease and now he’s working on developing a testing protocol for non-celiac gluten sensitivity that will be recognized by all.
Let’s Get Back to That Celiac Snob Thing …
When I spoke at the Canadian Celiac Association Conference in Toronto last June on Emotions in Motion: Psychosocial Effects of Gluten Issues, there was a question from the Q & A session afterwards that addresses exactly what this post is about, although I had started writing this post long before my presentation. I had not addressed celiac snobbery in my presentation, but the attendee’s question and follow-up discussion showed that celiac snobbery is indeed an issue for many. One of the audience members said:
“I was never tested for celiac disease, but I can’t eat gluten at all. How do I deal with others who have celiac disease who look down on me and don’t believe that my gluten-free needs should be taken seriously?”
I felt my face flush and my blood start to boil a bit when I heard her words. Not because I was offended by her question. No, that was not it at all. I felt a rush of emotions and an immediate churning in my gut, because I knew exactly where she was coming from. And so did lots of members of the audience. There were many nods and murmurs from other members of the audience. They understand. They’d been there. We’d been there.
Other individuals who had been diagnosed with celiac had dismissed their concerns and said things to them like, “at least you don’t have celiac” or “I have celiac disease so I really have to be concerned.” In any discussions, these others were likely to include terms to describe themselves like I’m a “biopsy-proven” celiac, “real deal celiac,” “card-carrying celiac,” “bonafide celiac,” “seriously celiac,” “full-blown celiac,” or “gold- standard diagnosed celiac.” Or I have “legit celiac disease” … and the list goes on. Those are all descriptions I’ve heard or read online, ones that many who have celiac disease like to beat others over the top of the head with.
The doctor of a friend of mine, a holistic practitioner, gave my friend a “de facto” celiac disease diagnosis. The doctor’s diagnosis was based on a supervised elimination diet, the friend’s particular array of symptoms, and the friend’s very positive response to the gluten-free diet (including a disappearance of other issues experiences for years). This friend, who is well known in the gluten-free community, says “they” are celiac, despite having no traditional testing of any kind. Was this friend’s doctor right? Probably. Admittedly, close gluten-free friends and I will hear symptoms of friends and family and pronounce our own “celiac” diagnosis. These friends and family of ours might go down the same road with a doctor as my well-known friend, but the word “celiac” might never be used or they might be told they are “simply gluten sensitive.”
Note that I am not bringing up this friend’s history because “they” discriminate against those with non-celiac gluten sensitivity in any way. They are an advocate to all who are gluten free. I just want to share the different paths that folks go down and the different labels they receive based on their doctors and their own labels.
There are actually many others in the gluten-free community who call themselves celiac, but are not “gold-standard celiacs.” Some had no testing of any kind as cited in my friend’s case above. Others had a positive blood panel, but didn’t choose to go through with the biopsy or couldn’t go through a biopsy due to cost or circumstances at the time. Others were given a celiac diagnosis after the blood panel only. Most individuals who had a positive blood panel, but negative biopsy don’t even call themselves celiac because they’ve been told by their doctor that they don’t have celiac, that such a diagnosis would not be accurate without a positive biopsy. And that’s true even when these individuals also have seen their symptoms resolve on a gluten-free diet.
Does all this matter? Clearly, it does, when the labels are being used inconsistently and in a discriminatory, ostracizing way by some. When anyone has medical issues caused by gluten—whether they have been diagnosed as a gold-standard celiac or not—needless to say I’m thrilled for them when they adopt a gluten-free diet. But I really wonder about the labeling that we’re using in the medical community, how fair it is, how accurate it is, and whether it truly serves the best purpose in the long run. One person is calling himself/herself celiac with no testing at all while another calls himself/herself non-celiac gluten sensitive and, quite frankly, gets treated badly and just catches overall crap for not having a “bonafide” celiac diagnosis.
I honestly feel like our current labels for gluten-related disorders (Dr. Fasano’s term)—and how they’re perceived and used—deceive, divide, and do little good. Others like Dr. Rodney Ford use different terms, their own terms. His term, “gluten syndrome,” is designed to be all encompassing with issues related to gluten. But use that term and people look at them like they’re bonkers. “Gluten syndrome? There’s no such thing they say.”
My friend Tom Malterre, MS, CN, of Whole Life Nutrition, says:
“Celiac disease is gluten sensitivity that has progressed to villous atrophy sufficient for the gold standard diagnosis.”
Think about that a minute. Yes, everyone who has celiac disease is gluten sensitive, but their disease has progressed to the point that there’s enough intestinal damage to test positive via biopsy and meet the gold-standard diagnosis. However, the catch here is that many who are gluten sensitive will never develop celiac disease.
If you’re a celiac snob, you think “Ah ha, got you!” But the medical professional experts in the gluten-free community will also tell you that so many of their patients who are non-celiac gluten sensitive come to them far more ill than their patients who test positive for celiac. What does that mean exactly? Does it mean that our current testing is lacking? Does it mean that our current definitions of gluten-related disorders are lacking?
One mom stated online in regard to her very ill daughter that:
“They couldn’t diagnose her with celiac because her villi weren’t damaged enough.”
Yet when her daughter went gluten free, all her health issues disappeared. I have some members of my gluten-free support group who fit the same category of having villi that were not damaged enough for a celiac diagnosis. One learned of a note in his medical file—“patient shows partial villous atrophy”—from his previous gastroenterologist only when he went to another doctor years later and finally, thankfully, got a celiac diagnosis. Another one of my support group members was told by her gastroenterologist that she had “some villous atrophy, but not enough to constitute celiac disease.” What was her doctor’s advice?
“Eat gluten until you have diarrhea and then cut back on gluten.”
Yes, that was the advice to one of our support group members from a local gastroenterologist.
Is that crazy talk or what? Some would consider it malpractice. Others would say that her doctor is appropriately following the guidelines for celiac disease diagnosis today. Dr. Tom O’Bryan says celiac testing is not very accurate unless there’s total villous atrophy. In those cases, he says, “it’s very accurate.”
So What Did I Say in Response to the Question at the CCA Conference?
I immediately acknowledged that I knew exactly what she was talking about. Then I asked for a show of hands of folks in the audience who were gluten free but did not have a celiac diagnosis. I followed that question up by asking how many of those folks had experienced what this attendee was referencing. The majority of folks in attendance did not have a celiac diagnosis and most of them indicated that they had experienced a similar, disheartening lack of support and “approval.”
I told the attendee and the audience that I had never been officially diagnosed with celiac disease either. I explained that after a lifetime of issues, I had been diagnosed with non-celiac gluten sensitivity and directed by my doctor to immediately go on a gluten-free diet versus undergoing gold standard celiac testing and waiting to see if I tested positive by those standards. I explained that my doctor at the time, who had been diagnosed with celiac disease via the “gold-standard” testing herself, felt that I was so ill that there was no time to waste. My doctor also felt that celiac testing was very inaccurate and the parameters for a diagnosis so narrow that I should not wait to see if I *might* test positive.
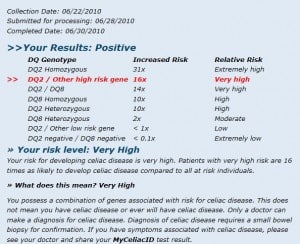
I told her and the audience added that I had later had celiac gene testing done and determined that I did have celiac genes and it was clear from the changes in my health and the results when I get “glutened” that gluten-free living was the right health choice for me—with or without a gold-standard celiac diagnosis. I also admitted that I was glad that I had not been diagnosed with celiac disease, not because I thought that a celiac diagnosis would indicate that my gluten issues were more serious than they are without a celiac diagnosis, but because I *might* have become a celiac snob had I received that definitive diagnosis.
You see for many years, I was more of a “black and white person,” per se, and bought into everything that my doctors and the medical community said even though it was inaccurate. I believed that I had irritable bowel syndrome or a nervous stomach because that’s what I’d been told. I believed that my health issues ran in the family. I believed that stress was often the main cause of my issues. Many of you reading have been down the same road and led to believe the same things only to learn later that you had celiac disease or serious gluten issues without celiac disease, now referred to as non-celiac gluten sensitivity.
I’ll admit that I have never been crazy about the term non-celiac gluten sensitivity. Understatement. First, there’s the “non-celiac” part. Hey, you’re not part of our group. Second, there’s the “sensitivity” part that bothers me. It implies that our gluten issues are benign, minor, that there’s some level of tolerance, that we’re simply sensitive to gluten. In other words, the presumption is that if we eat a little gluten, it’s not a big deal. For most of us who do not have a celiac diagnosis and by default have received the non-celiac gluten sensitivity label, this presumption couldn’t be further from the truth.
I advise anyone who has ANY gluten issues not to eat gluten in any amount. Ever. Personally, I cannot tolerate even small amounts of gluten. I react to far less gluten than the FDA has approved to be allowed in products that exhibit a gluten-free label. (The FDA law of less than 20 parts per million in any product labeled gluten free goes into effect August 2014.) But not everyone notes their own reactions to gluten and our bodies can be reacting without visible symptoms. But that’s a discussion for another day.
I told the audience that part of the issue with not being taken seriously and being supported when living gluten free without a celiac diagnosis was that the term “gluten free” has become a media buzz word. Journalists, comedians, and other celebrities are using the term gluten free as the word “du jour” to get attention and readers/viewers.
“Gluten-free mostly” or “gluten free when I want to be” tends to describes many of the celebrities’ eating plans. Most of you reading know what I’m talking about. Many tv shows and movies have at least one mention of “gluten free” now—and they’re not usually positive mentions.
We need to focus on facts though. Listen to Jules’ (GF Jules) interview on The Gluten-Free Voice with Dr. Fasano and hear his thoughts on the study I mentioned earlier, including some important data on that study that hasn’t been widely shared, as well as his statements on the differences between celiac and non-celiac gluten sensitivity, and much more. The show is definitely worth a listen!
A Little Bit More on The “Gluten-Free Diet Du Jour” Causing Us Issues
On one of our many trips, Mr. GFE and I met reader friend Dena for dinner a few years ago. We had a delicious and safe gluten-free meal and ended up chatting with and thanking the chef on the way out. He told us that he regularly has folks come in and order a gluten-free meal and then order a gluten-full beer to go with their meal. Yes, you read that correctly. And these folks do this knowingly. By choice. The restaurant staff determined this was the case when they made further inquiries concerned that the diners were not up on their gluten knowledge and unknowingly consuming gluten. Oh, no, they were told, “I want a gluten-free meal, but I am fine with drinking gluten beer. I am not that sensitive.” Grrrr.
The chef expressed his frustration in going to great lengths to prepare safe, gluten-free meals in a “dual” kitchen for folks who end up not even needing a gluten-free diet. We totally understood his frustration. The fact is these types of folks who don’t eat 100% gluten free “muddy the waters” for the rest of us and making dining out less safe. Just last week I was told by a restaurant with a gluten-free menu that they would handle my food differently since they knew I “truly needed to eat gluten free.” So the “gluten-free menu” at that spot doesn’t really mean gluten free.
My final statement to the attendee and the audience at the conference was, “We need to realize that we are all in this together and we should be supporting each other versus questioning our diagnoses.” And I believe that wholeheartedly. We all need gluten-free friends. Folks who get our issues, who know how to feed us, etc. Let’s make more of these friends and support each other and let the medical community figure out the rest.
I don’t want to get into a discussion on folks advising others to go back to eating gluten to see if they actually have celiac. To me that’s even more “crazy talk” and that’s not what this discussion is about. Today’s discussion is about acknowledging that there are folks eating gluten free for health reasons without a celiac diagnosis and they deserve the same acknowledgement and respect as those who have a celiac diagnosis.
Others call themselves celiacs although they’ve never gone through testing, in some cases, they’ve had no testing at all. Sometimes these are folks who have a family member who has been diagnosed with celiac disease and they see they have the same symptoms and call themselves celiac. Who knows if they are truly celiac or not? Do we care? We do care if they are not taking their gluten issues seriously and continue to eat some gluten. As I already stated, these part-time gluten-free folks confuse matters for the rest of us, plus they’re undermining their own health.
Have I ever stated that I have celiac disease? No, but if restaurant servers or others in passing assume that I have celiac disease, I don’t correct them and go into my medical history. It’s easier to leave it at that. The end result is the same. I need truly gluten free food or I will get ill.
What happens when celiacs, particularly celiac snobs, have a child who does not test positive for celiac, but clearly does not thrive while eating gluten? Being a mama bear can change the whole dynamic and perception of who should be gluten free and whether one needs a celiac diagnosis. Does it make sense that a mom is celiac, and one child tests positive for celiac, but the other is “only” considered gluten sensitive because s/he continues to test negative for celiac? How many times have you seen that? Being a gluten-free support leader and active in the gluten-free community, I’ve seen it A LOT.
Remember that celiac testing only offers a negative result at that point in time. The family members of many celiacs I know are tested at least every other year via blood panel to see if they have developed celiac because of the high incidence of celiac in families as it is a genetic autoimmune disease. If the child received a negative blood panel after their mom or dad was diagnosed as celiac, were they told “okay, that’s it, you don’t have celiac. You’re good for the rest of your life!” Yes, unfortunately, some have pretty much been told that, but celiac disease really doesn’t work that way.
Yet, folks are being told that if they have issues with gluten, but don’t test negative for celiac disease that they have non-celiac gluten sensitivity. And the implication is that this diagnosis is forever. Really? I don’t think so. How many people do you know who had problems for years, even testing negative for celiac more than once before they were diagnosed as celiac? Obviously, this is not a “black and white” topic at all.
Okay, readers, what are your thoughts? Are you a gold standard diagnosed celiac? (If you have been diagnosed celiac but did not test positive on the blood panel AND biopsy, please tell us more details of your diagnosis.)
If you are gold standard-diagnosed celiac, do you take the needs of others who eat gluten free for their health, but don’t have a celiac disease, seriously? NOTE: I’m not talking about others how eat gluten free depending upon the direction of the wind that day; e.g., some Hollywood celebrities. I don’t take them seriously either.
If you have not been diagnosed with celiac disease, but are eating gluten free for health reasons, please tell us why (briefly or with as much detail as you’d like to share).
If you are gluten free without a celiac diagnosis (and you don’t call yourself “celiac”), have you felt looked down upon by other celiacs or celiac organizations? Do you hear the word “celiac,” “celiac,” “celiac,” from some organizations until they want your donations and then suddenly it’s all about “gluten free” vs “celiac”? I have certainly seen that occurrence year after year. Some organizations have even admitted off the record that celiac disease is what gets the attention and the dollars.
Thank you for being willing to take part in this important discussion!
![I'm Celiac You're NOT. I could have been a celiac snob. Don't be a celiac snob if your diagnosis is gold-standard celiac vs non-celiac gluten sensitivity. Everyone who eats 100% gluten free should be accepted. [from GlutenFreeEasily.com] I'm Celiac You're NOT. I could have been a celiac snob. Don't be a celiac snob if your diagnosis is gold-standard celiac vs non-celiac gluten sensitivity. Everyone who eats 100% gluten free should be accepted. [from GlutenFreeEasily.com]](https://glutenfreeeasily.com/wp-content/uploads/2014/05/Im-Celiac-Youre-NOT.jpg)


Zippy says
Bravo! You said everything that I’ve been saying. Many people can only diagnose themselves because the medical community fails them. Most take a decade or longer of being seriously ill before they figure it out for themselves. Of course the ideal is to get a definitive diagnosis, but that is with the assumption that they can find and/or afford to do so. A co-worker has a son with Celiac symptoms. After three years he obtained insurance and was able to see a specialist. The gastroenterologist did a colonoscopy..that is it. No upper endoscopy was scheduled. No Celiac blood panel ordered. He proudly told him he did not have any of the “three c’s — cancer, Celiac, or Crohn’s. He said he had symptoms due to food poisoning which occurred three years AFTER his first bouts with debilitating diarrhea. He will continue to eat gluten. It will continue to probably kill him. This isn’t an isolated story. This is sadly the norm for many areas. So to the Celiac snobs..be happy that you had medical care to diagnose you. Most aren’t lucky enough to have it explored.
Shirley says
Hi Zippy–First, welcome to gfe! Second, thanks so much for your comment, as painful as relating and hearing those details is. I agree with you that medical community is failing to diagnose folks with gluten issues, and on an epic scale. Every single doctor who uses a colonoscopy as a means to diagnose or exclude celiac disease should be brought before the medical board. When a disease is diagnosed from damage to the small intestine, it cannot be diagnosed by examining the colon. Duh. Any layperson can figure that out. Yet I have had friends, family, and support group members tell me the same thing over and over again though. “I had a colonoscopy and my doctor told me I don’t have celiac disease.” Malpractice plain and simple. And because most folks don’t want to have celiac disease (and/or have blind faith in their doctors), they won’t pursue getting proper testing or calling the worthless doctor out, so to speak. There are very obvious other disconnects in your friend’s story and others’ as well. But that blind faith and lack of knowledge (and lack of wanting to truly know in some cases) on the patients’ part is keeping them from connecting the dots. I hope some miracle happens for your friend, so that he does get diagnosed and goes gluten free. I agree that those who have a true diagnosis have been given a gift in getting that validation/”an answer” that most of them might not fully appreciate.
Thanks again!
Shirley
Ina Gawne says
Shirley – this is such an insightful article…thank you! I have never been tested (thank god…if I’d waited I might be dead) I call myself a celiac because my reactions are so SEVERE. One crumb, and I am blistered from mouth to my entire stomach/intestines. It can take up to 4 weeks to recover. Regardless of being a celiac or gluten sensitive it makes no difference to me…if you get sick from a food – one must immediately stop eating it. I too went through the same rigamaroll that you did with Doctors – IBS, cut down on the stress level etc.etc. 25 years of that nonsense before I finally (on my own) went GF. Now, I take absolutely no chances when it comes to eating gluten free safely. I hope one day the testing will become easier and whether one is sensitive or a celiac the results are still brutal aren’t they? Thank you for your wonderful insights and for sharing with all of us!
Shirley says
Thanks, Ina. It’s always wonderful to hear from you and get your input! What you said is true for so many of us. We’d probably be dead if we hadn’t gone gluten free without a celiac diagnosis. I’ve personally seen folks who have been disabled to the point of being in a wheelchair before going gluten free on their own or with the help of a more enlightened doctor. Crazy how our paths were so similar, but when you compare personal stories with others, you find differences for sure, but also a lot of the same similarities. I’m so glad that you learned what was causing all your issues and reclaimed your life. Sometimes I think about what my future would have looked like if I had not gone gf and I see others headed down the same road and it’s so painful. We’ll all keep working towards the better testing, better education of doctors, teaching friends and family to be their own advocates, etc., so that one day so many will not fall through the cracks!
Hugs,
Shirley
Cheryl Harris says
What a fantastic post, Shirley. The NCGS hype has been crazy–the study has been out for months, and now the media is turning it into a circus. Does it really matter if the bagel is causing pain because of gluten or if it’s because of the fructans in wheat? bagel=pain should suffice for the general public. oy.
Shirley says
Thanks so much, Cheryl. Your positive feedback really means A LOT to me! The frenzy continues this week, too. It’s really sad how hard those of us who have found our answer have to fight to get acceptance/not be the focus of jokes, etc. Yes, indeed, “bagel=pain should suffice for the general public” or anyone really. It’s like the old joke about the patient saying to the doctor that when he bangs his head against the wall, it hurts and asks the doctor what he should do. The doctor says stop banging your head against the wall. For those of us who know that gluten is our issue—our head banging against the wall—we can just stop the banging—eating gluten. We shouldn’t need anyone’s approval or validation for that.
Shirley
Vicky says
This is an excellent post Shirley which I will share on my facebook page, thank you for touching on a topic which I think many of us have been exposed to.
My endoscopy showed no damaged villi and therefore in the UK, I did not have Coeliac Disease, it’s very black and white in the UK. So I went away with a diagnosis of IBS and a leaflet.
While my husband and I were travelling in the car today (for miles just to buy some organic vegan gluten free sausages, lol), we were actually discussing this very topic since my husband has been gluten free for a year too.
Since I haven’t been diagnosed, why do I follow the diet? Well the truth is I no longer have IBS and my thyroid medications have reduced significantly – enough said!
I don’t particularly care what people think about my diet and I’m sure many do comment behind my back. All I know is my health has improved without gluten in my diet. I don’t know any diagnosed coeliacs but I know many people who have adopted this lifestyle and feel better for it. However, I have felt looked down upon by some people online but I won’t go into that here!
Thank you for your “ramblings”, this was very interesting and very enjoyable to read!
Vicky xo
Shirley says
Thank you, Vicki, both for the kind words and sharing your family’s personal story! It’s really hard to understand 1) why we have to wait for end-stage disease before it can be diagnosed and 2) why folks—even doctors—want to disparage anything that causes us such health improvements. We do have to have our own convictions that what we are doing what is right for our own health and not waver in our dedication to our healing diet. I share ramblings like this one because not everyone has that conviction yet. I hope they can eventually give it to themselves though because waiting on validating through the medical community will be a long time coming.
Thanks for sharing this post with others, too! xo,
Shirley
Hannah says
Thank you for this! I have not officially been diagnosed but I know that my symptoms from being glutened are on par with or even more severe than the people I know with actual diagnose celiac. I never got tested because I had already gone gluten free and after hearing my reactions to gluten and how much my health improved after going GF, my doctor refused to test me. He said it wasn’t worth the risk to my health, especially since there was no guarantee I would even get a positive result. I have finally gotten to the point where I just tell people I have celiac because it is annoying having to explain and justify why I’m GF. It amazes me how rude people are, especially those who knew me before I went GF a couple years ago because of how quickly I made the transition. Thanks again for the article!
Shirley says
Hi Hannah–Welcome to gfe! 🙂 I really appreciate you taking the time to comment and sharing your story. I’m so glad that you’re gluten free and healthier, no matter what label you do or don’t have. Your doctor is SMART IMO. I know that many feel they need that validation though and others say testing is needed for future medical concerns, stats, etc., but you would live the same either way as your doctor says (if you have the conviction to stay gf; some do not unfortunately). It’s very hard to understand why folks would question a way of life that has made you so much healthier, isn’t it? But it happens so often—with skepticism coming from the gf and non-gf individuals. Whatever, right? Live on gluten free and healthy!
Shirley
Trish Parker says
I have not been diagnosed celiac but have been gluten free since August of 2013. I made the decision to go gluten free to try to reduce debilitating inflammation due to osteoarthritis. After a month of no gluten, I realized that my chronic diarrhea was gone and so were the unexplained itchy rashes that had been diagnosed as stress related by several doctors. After six months of being gluten free I realized my arthritis was actually better and in fact, I felt better everywhere. I do encourage anyone who wants to try removing gluten from their diet to get support. Without Shirley and the Gluten Free Easily Group, I would have given up before I got results. No one in this group makes a big deal about whether you are a diagnosed celiac sufferer or just gluten free by choice. Thanks again Shirley for all you do to keep us healthy all the time!
Shirley says
Hey Trish–Thanks so much for both your comments! I appreciate you sharing your personal story. Dr. Rodney Ford says that “gluten syndrome” (his term to cover all gluten issues) primarily affects brain, skin, and gut. And as you share and as many others have seen (myself included), it can also affect joints. Gluten is inflammatory so many of our symptoms can be related to that inflammation and while inflammation, like “sensitivity,” sounds rather benign, it can be anything but. I’m so glad that our group has been so helpful to you and that you’ve received nothing but support from Day One. I applaud your doctor, too. You didn’t mention it here, but I think it’s very telling that—as you shared with out group—when your doctor herself went gluten free, she didn’t see a need to get tested for celiac. She eliminated gluten and got better and then reintroduced gluten and got worse, so she removed it from her diet again … forever. I’m so happy for anyone who figures out the gluten connection and receives healing via just about any path.
Thanks again, dear!
Shirley
Jen says
Glad I found your site…especially right now. I am pretty sure I a gluten intolerant because of these “attacks” I have been having….and I have been doing my due diligence of reading up on blogs and all sorts of gluten information and taking what is relevant to me and learning. As I am typing this I am being attacked by something…gluten is probable here. It came in last night after eating pad thai….rice noodles ok….and i took out egg as well because I can’t eat egg yolk anyway….after eating some of it I started having slight pains but kept eating anyway….decided to stop and then about 45 minutes later ate more and then it hit me…..the painds in my stomach…the salivating and nausea…the tightness in my jaw and the bloating of my stomach….I went home and got in bed right away….thank god I fell asleep.
This morning I awoke and was feeling a bit better but pain came back a few hours later and then subsided and about 30 mins ago came back again….this time raging….nasuea, salivating, abdominal pain, bloating, chills…..
I drank tbsp of apple cider vinegar with water, I have some tea by my bed side and a glass of water…..
this pain is bad and I feel like I have been food poisoned…literally! Ugh……I need a diagnosis ….STAT. Soon I am going for blood work and will be seeing a naturopath…sooner needs to be here NOW rather than later.
: (
Shirley says
Hi Jen–Welcome to you! I’m so glad that you’ve found my site, too, and are figuring out some answers for yourself. I appreciate you taking the time to comment. But I’m so very sorry that you’ve been glutened. Pad Thai can have gluten it in via other things than the noodles. Soy sauce that contains gluten (in the form of wheat) is the most usually one. I have a post on recovering from being glutenedfor future reference. Good luck with all your testing. I do recommend official celiac testing, but if the results are negative, don’t consider that a free ticket for eating gluten.
Again, good luck and hugs to you!
Shirley
Molly (Sprue Story) says
I was diagnosed via the “gold standard” and have probably at times been guilty of celiac snobbery, but I try to actively work against any reliance on my “celiac privilege.” As with any other kind of privilege, sometimes we might say something that isn’t intended to ostracize but that still makes others feel left out. That’s why I’m a fan of the umbrella term “gluten-related disorders,” which includes us all (even if it sounds a bit stuffy/technical).
I do, at restaurants, state that I have celiac disease when asking the kitchen to be extra careful, but this is not intended to be in contrast to those who are gluten sensitive but rather in contrast to that percentage of people trying to eat gluten-free who don’t really get what it means. That sometimes backfires when the waiter/waitress clearly doesn’t know what celiac is, and I then go on to say “it just means I’m really sensitive to gluten” and they in fact get that much better!
The “NCGS isn’t real” madness drives me insane and I wrote about it on my blog this week too. I’m sure it must be even more upsetting to those of you who aren’t “lucky” enough to have at least that one line in each of those absurd “articles” allowing that OUR disease is legitimate. I’m sorry, guys. I hope it will blow over soon because the Internet has a very short attention span.
Shirley says
Hey Molly–Thanks so much for taking the time to weigh in on this discussion! You raise a very good point and I actually had that discussion the other day on my personal FB page the other day. So often, folks go with what they know. So those who are diagnosed as celiac often have not even heard of NCGS. Sometime they do learn about NCGS later, particularly when they find out a family member/friend has the issues, but doesn’t fit the celiac parameters. There are so many terms to “label” our situation and so many ways to express it to others to explain ourselves, mostly to keep up safe when dining out as you shared.
I saw another crappy article today, so I don’t think it’s blowing over too quickly. It’s like the old expression, they’re like a dog with a bone and won’t let it go. A new study could come out tomorrow completely discrediting everything in the last one and the info and articles would still live on. Misinformation and sensationalism never seems to die on the web. 🙁
Thanks so much for your support of those of us without a celiac diagnosis! Must check out your post!
Shirley
M
Lyn says
I have not be diagnosed with Celiac but have had lab work done with positive results for Celiac genes and other results that highly indicate I have a problem with gluten. The only reason I haven’t had an endoscopy is because I have already been GF for over a year and I am not willing to go back to gluten and the way I felt when I ate it in order to get the test. I don’t say I am Celiac when I eat out but I do stress that I get very ill if I eat ANY gluten. Most restaurants do not want their patrons getting ill in their establishments. Most of the time I have no problem but there are times when the wait service is very annoyed with me probably because I have a long list of other foods I also cannot eat because they are migraine triggers. The real test will come when I go overseas this summer and am hoping I can communicate my needs. Thank you for this article–as always it is very encouraging and helpful.
Shirley says
Hi Lyn–Welcome to gfe and thanks so much for taking the time to comment! I say do whatever works best for you to keep you healthy. Many (I don’t know the exact stats, or if stats exist) won’t test positive for celiac even after resuming eating gluten. The test is only accurate when there is significant damage and that takes time. During that time, exposing ourselves to gluten could trigger other autoimmune conditions. Obviously we don’t want that.
You’re so right that restaurants generally don’t want their patrons getting ill. We have to be firm, but kind with them—working together so we all get the result we need and want. As far as your overseas trip, I’d recommend checking out the resources on Gluten-Free Globtrotter’s blog. Erin has a number of posts sharing dining cards, apps, etc. We’re using the Gluten-Free Passport dining cards that she mentioned on her blogwhile we’re in Mexico this week. They’ve been a great help! Plus her whole site could be helpful to you. Hope you have a wonderful, safe trip! 🙂
Thanks so much for your kind feedback, Lyn,
Shirley
Cari says
Thank you, Shirley, for this excellent post. I have been doing a lot of reading about celiac disease and gluten intolerance (or sensitivity). I feel that, while they are technically not the same thing, both require the same dietary diligence and deserve the same amount of respect as medical issues.
Having just received a “gold standard” diagnosis of celiac disease almost four weeks ago, I have relied on a dear friend who is gluten intolerant for advice. In truth, I would never have had the blood tests for CD without hearing this friend’s symptoms and recognizing them as my own. My physician tried (twice!) to talk me out of the blood tests when I requested them because I am overweight. Words cannot express the gratitude I feel for my gluten intolerant friend, as I am sure that without her, I would never have been diagnosed.
I am also grateful that the people who opt for gluten-free diet without actual medical concerns have increased the demand for GF foods. Manufacturers are jumping on the bandwagon and labelling their products with easy to read GF labels. I do admit to snobbery when they cheat by drinking that beer with their GF meal!
Again, thank you for this article. It really helps to shine a light on the importance of perception as we walk the path to good health.
Shirley says
Hi Cari–It looks like this is your first time commenting here on gfe—welcome and thanks so much for taking the time to comment and share your very telling story! I totally agree that both conditions require the same dietary diligence and deserve the same respect.
Like you, many folks have not been able to convince their doctors to test them. The doctors who believe in celiac (yes, there are still doctors who actually tell their patients they don’t believe in celiac) are going by the “picture” of celiac from textbooks decades ago. That would be the very emaciated person. In actuality, most people who have celiac today are actually overweight, with normal weight folks being most common, and the emaciated folks only making up about 6% of celiacs (figure from a presentation by Dr. Fasano about 10 years ago). I’m so glad that your friend was there to help you in every possible way including inspiring you to get tested. Kudos to you for having the conviction to insist upon testing. If doctors would test every time instead of say “I don’t think you have celiac.” we’d certainly get a lot more folks diagnosed!
I like that there are more gluten-free products, too, but after learning to really reading labels—not only gluten, but for everything to see if I want it in my body—I want better quality products, not just gf. I hope that companies will step up to the plate on that.
I’m totally with you on not being able to accept the folks ordering a gf meal and then drinking a gluten-full beer. If they’re just eating “low gluten,” they can guess what’s gf and take more of a low-carb approach without evening bringing up the term “gluten free.”
Thanks for all your kind words, too!
Shirley
Yvette says
I have not been diagnosed with Celiac and have never even had a blood panel done. But I have suffered with stomach issues since I was an infant. My poor mom took to me to doctor after doctor and nothing really helped the symptoms. I just learned to live with them.
If I were going away from home I would just refuse to eat or miss out on the activity all together if I knew there would not be a bathroom nearby. Fast Forward to 3 years ago… I was reading an article about Celiac in a women’s magazine and noticed that I had many of the symptoms so I decided to give up gluten to test my theory. In about 3 months almost all of my symptoms disappeared, it was like I had a new life. I made an appointment with my GP and we discussed my experiment. He said there was really no need for the test because there was no cure I just needed to stay away from gluten. He said it didn’t matter what label I had if giving up gluten helped then that was all that mattered.
I still have issues occasionally but they are what any normal person would have. EX. Eating large amounts of spicy food. When I am around people I don’t know I just tell them that I can’t eat gluten because of stomach issues and they seem to except that explanation.
Shirley says
Hi Yvette–It looks like you are new here, too. Welcome! I can totally relate to your history of having issues from a very early age and never getting any answers. Bathrooms were key. I always knew where they were.
I’m so happy that you read that article! I’m also so happy that your doctor recognized that you had already implemented the cure and didn’t insist you go back on gluten. While I would like the diagnosis rate for celiac to go up (just to help folks, plain and simple), your doctor was acting in your best interest, which is very admirable and not too common.
I’m glad that you have not had any issues with other folks not accepting your gluten-free path either!
Thanks so much,
Shirley
Patti says
Hi, I don’t know if I have celiac disease, but I have a suspicion that I do, so I’ve been following a strict gluten-free diet for over 2 years now.
Looking back, I had a lot of weird, seemingly unrelated symptoms my whole life, as did my mother. I even wonder if my oldest brother, who died from lymphoma when he was in his 40’s might have had it.
Since childhood, I suffered from frequent stomachaches, canker sores, teeth abnormalities and then constant headaches, increasingly worsening joint pain, rashes, diarrhea, numbness and tingling in my arms, fingers, calves and feet, then in February of 2012, everything just blew up (as I like to say). In addition to all of those problems, I started getting severely bloated, where I looked like I was 9 months pregnant. After I started having tightness in my chest for the 3rd time in one week and thought that I might be having a heart attack, I went to the ER. They did tests for my heart and told me that everything was fine and that maybe it was just stress. The following week, when I wasn’t getting any better and felt like I was going to die, I went to another ER. They took urine and blood samples and told me that everything looked fine! They look at you like you’re crazy…like it’s all in your head. I was so frustrated and scared. I know my body, I know this isn’t right, that something is going on inside me. It was winter and I was about to leave for a week’s vacation in Florida and I did not want my vacation ruined because I was feeling so sick, so in desperation, I googled my symptoms and it brought up celiac disease. I had never heard of it (or gluten) before. When I saw all of my symptoms listed there, I decided to stop eating it and see what happened. My symptoms went away.
When I finally got an appointment with a gastroenterologist, and he scheduled an endoscopy, I said, “I guess I need to go back to eating it before the test” and he said “No, just keep doing what you’ve been doing” I have no idea why a doctor would say that, did he not believe that I was totally avoiding gluten? Did he think that I was cheating? So, when I had the endoscopy, I hadn’t been eating gluten for over 2 1/2 months. They called me the following week and said, “We didn’t find anything significant in your intestines, so you don’t have celiac disease.” I thought the way they worded that was odd. Someone in the local celiac community later told me that some doctors don’t know how to read the results correctly, that they think the villi has to be completely flattened to confirm a diagnosis. Now, even though I would like having the diagnosis, if I do have celiac, I don’t know that I can go back to eating it to get tested again, because on the rare occasion when I accidentally get glutened now, I feel horrible for days.
As for “celiac snobbery”, I don’t think I’ve experienced that too often, but at one point I thought that I ought to see a dietician for guidance, since my gluten-free diet might be lacking in certain nutrients and when I spoke to someone from the “Celiac Center” at a local hospital, I was told that I couldn’t see their dietician unless I was diagnosed with celiac.
Sorry for such a long post. I really enjoy reading all the gluten related blogs and other people’s stories, but this is the first time I’ve
posted. Thanks.
Shirley says
Hi Patti–I really appreciate you sharing your personal story with us all and would like to officially welcome you to gfe! Many of my gluten-free friends and I have commented on how we can look back at our family tree and see so many others who likely had gluten issues. Lymphoma, specifically, is very often related to undiagnosed celiac. I am so very sorry for the loss of your brother.
Your own history definitely points to a “gluten-related disorder.” It does sound like the doctor and other folks interpreting your testing results saw damage, but not enough to constitute celiac disease by today’s definition. You could probably ask for your results even now and see exactly what they saw, or at least what they noted. It might be more than that summary they gave you on the phone. But the bottom line is that you know that gluten is poison to your body and steering clear of it 100% of the time is required for your health.
Thanks for sharing the fact that you couldn’t be seen the dietitian at the celiac center, too. I’ve heard that before and I think that’s disturbing that one has to have a celiac diagnosis to get help on living gluten free.
Thanks again, Patti, and, btw, there’s no such thing as too long a comment IMO. Our personal stories and perspective can’t be shared in just a few words.
Shirley
Trish says
Here is how I was “diagnosed”…After several encouraging discussions with Shirley, I took a stool test from Enterolab. The results showed I did indeed have severe gluten issues. I took the paperwork to my primary care physician, who is gluten free herself, and she confirmed that I should never eat gluten again. Surprisingly within sixty days my mysterious skin and digestive issues showed significant improvement. Who knows how long it would have taken me to figure out that it was even gluten causing my problems, because I originally stopped eating gluten to try and reduce inflammation from osteoarthritis!! I had no idea of what the symptoms were for gluten intolerance. I was just willing to do whatever I could to reduce my pain. Six months later the arthritis pain decreased as well. I have had no celiac snob issues. Everyone I have come in contact with has been very supportive.
Audrey @ Gluten-Free Vegan Love says
I am not a diagnosed celiac. I’ve done the blood test and a biopsy and both came back negative, but the symptoms were clear to both myself and my doctor who said I must just have a very strong gluten intolerance. To be honest, the official diagnosis didn’t mean much to me, since it only helps to identify such a small fraction of gluten-related disorders that it didn’t seem to matter. I know from clear experience that I can’t continue eating gluten and expect to be healthy. Ultimately my experience matters much more to me than a piece of paper saying something about me based on someone else’s criteria.
On the note of my test, one thing I can say is that my test was certainly not handled properly. My doctor told me to go off gluten, and then a few months later when I was undergoing other tests he said I may as well do a celiac test while I’m at it. He then realized I’ve gone off gluten (as per his instructions) and told me I would need to start eating gluten again for some weeks prior to the test (one of the most awful few weeks of my life, as you may imagine), though he said the results won’t be as accurate now because I had a period of being gluten-free. I’m not sharing this to justify or claim that maybe I have celiac after all, but just thought I’d share the very likely possibility that people can easily get misdiagnosed even due to situations like this.
I’ve never actually experienced celiac snobbery from celiacs. But I do notice a difference from people who aren’t gluten-intolerant towards how I explain why I can’t eat gluten. I think people are so conditioned to think gluten-free is a fad that they have a hard time accepting you may just actually be gluten-intolerant. Now, if I was to say I’m celiac, that would be a whole ‘nuther story. They take that far more seriously. I usually tell restaurants I’m not familiar with that I have allergies and will get VERY ill if I eat gluten (and some other ingredients). I just need the peace of mind knowing they will take my concern seriously (or at least I’ll know from their response that perhaps I shouldn’t be eating there at all).
Shirley says
Hi Audrey–Thanks so much for sharing your personal story with us all. I really appreciate it and I’m glad you’ve found the path that works best for you without having that gold-standard celiac diagnosis. The “path that works best for you” is the most important thing I think. And, yes, I believe it’s all too easy for folks to get misdiagnosed. I’m hoping that we see phenomenal improvements in the near future—including a broader, all-inclusive definition for serious gluten issues and testing that’s incredibly accurate for seeing all damage.
The fad thing is definitely hurting our cause. Like you, I caution folks that I get very ill. Unfortunately I still get glutened occasionally as folks in restaurants, etc. don’t truly understand the scope of what gluten free means. We’re on vacation this week at a resort where Spanish is the primary language and with us not really speaking Spanish and me being gluten free and Son being gluten free and dairy free, we’ve sent back quite a few dishes. The resort dining room/kitchen personnel have been very gracious though because they want us to be pleased and not get ill. We’re at the very end of our vacation and they’re finally getting our meals right now.
Shirley
Amy says
My daughter has celiac disease, and I fully respect those that label themselves non-celiac gluten sensitive. I believe if a food is bothering your system and it helps to cut it out…more power to you! A few comments though:
1) It is important to have “traditional” diagnosis w/ blood test/biopsy, etc. B/c w/ range of drug treatments being tested, they may be applicable to those w/ celiac but not gluten sensitivity.
2) I agree w/ the chef’s feelings about those who order a gf meal, then cheat or are ignorant. As well, there are a lot of places that advertise GF pizza, for example, but there are big cross contamination issues. I know Gluten sensitive people who can tolerate it, but it’s not for my daughter. So I get the stink eye that I’m being overly cautious/difficult, etc., when we won’t eat at such places.
3) At a wedding recently I sat at a table w/ a man who is gluten sensitive. He sat near me and ate a bowl of soup w/ barley. I have no tolerance for people who spout they are gluten sensitive and then blatantly eat gluten. It hurts the efforts I have to go to to make eating out safe for my child.
Audrey @ Gluten-Free Vegan Love says
Hi Amy,
I didn’t think of the celiac test as being useful for drug treatment when I wrote my comment above (re: official celiac diagnosis having no meaning for me), but you are right that it may be helpful to some. I guess since I don’t take any drugs in my case, the idea didn’t occur to me when writing that. Thanks for pointing that out.
Shirley says
Hi Amy–Welcome and thanks for your comments! I am glad that you are “all inclusive” as far as those who eat strictly gluten free for health reasons.
1. I think the differences between celiac and non-celiac gluten sensitivity are not fully established, but I certainly understand that drug and vaccine trials are geared towards celiac disease because it is more defined. Even if I personally am not gold standard-diagnosed celiac and never plan to take any drugs, that is an important point for those who would consider drugs.
2. That is not the first time I have heard a chef’s or restaurant owner’s frustration with “wishy washy gluten free” patrons. I don’t believe that any gluten sensitive folks can really tolerate gluten. I just believe their symptoms might be different or not as pronounced. Their bodies still might be screaming albeit silently at least until they can’t take it any more and protest by manifesting other serious diseases such as cancer or new autoimmune conditions. The longer one is undiagnosed and/or continuing to eat gluten, the more likely they are to get additional autoimmune conditions.
3. I agree with you. I have no tolerance for those folks.They hurt all of us who are truly gluten free. While I realize that many individuals have to come to a realization on their own that they need to be 100% gf and can’t cheat, they should not be using the term “gluten anything” to describe themselves. that’s why I really don’t like the “sensitivity” part of the NCGS term. It implies a tolerance that is not there in my and many others’ opinions.
Thanks again,
Shirley
Olivia says
Such a great article.
I’m one of the unlucky people with celiac. It hit me hard, too: irreparable systemic damage, an endless list of food and topical allergies + various autoimmunities, the list goes on and on. The list of foods that I CAN eat is way shorter than the list of foods that I can’t. My body even reacts to vitamins, so I’m in a constant state of deficiency.
One thing I’ve never understood is gluten-free and celiac snobbery. If gluten negatively affects a person, then whether the issue is celiac or a sensitivity shouldn’t matter. People on both sides need to avoid it.
On the flip-side of the snobbery scale, if a person has no issue with gluten or wheat, why avoid it? It annoys me when totally healthy people talk about being gluten-free and act like they’re so much better than everyone else.
After the hell I’ve been through and will continue to suffer, I wouldn’t wish this disease on anyone. And how stupid to think that having celiac trumps gluten sensitivity. One may be worse in terms of the physical repercussions, but it’s awful to belittle someone’s health problems no matter its relativity to yours.
To those of you with gluten sensitivity, hang in there! People who play the “I’m Sicker Than You Are” game are ridiculous. Your health issues are valid!
Shirley says
Hi Olivia–Welcome to gfe! Thanks so much for the kind words on my post and leaving such a thoughtful comment. Well said on all!
I’m not sure how long you’ve been gluten free, but I will tell you that the list of foods does grow tremendously, even if one has other sensitivities. For many of us, there still continue to be other issues though and that makes everything hard to navigate at times. 🙁 As you’ve said, we wouldn’t ever choose this condition. I’m not opposed to folks eating gluten free if they prefer, but when some order a gluten-free entree and then get a gluten-full beer to go with it, the “muddied waters” make it much harder for all of us who are truly gluten free. “Gluten free” should mean “gluten free.” If a person wants to eat less gluten, they can simply order the items on the menu that are naturally gluten free and not worry about cross contamination like we do or they can pick the croutons out of their salad. Just don’t call the eating that you’re doing “gluten free.”
Admittedly being gluten free has brought me many blessings (e.g., making so many gluten-free friends; knowing what is in all the food I’m eating; adding so many more whole, real foods to my diet) over time for me though and I’m so grateful for them.
I’m so glad you’re not into the snobbery, Olivia, and I totally agree on how unnecessary and ridiculous it is to play the “I’m Sicker Than You Are” card. I’ve never heard it called that before, but that is such an accurate description.
Thanks again, Olivia.
Shirley
Rebecca says
Thank you for this post. My blood test for celiac came back negative after a horrific gluten challenge a couple of months ago, and it was such a relief to return to my gluten free ways. I used to use my mother’s kitchen (my kitchenette has only a toaster oven, and no space for other small appliances) to make my baked goods, until I learned about cross contamination. It went a long way toward explaining why I got sick after eating supposedly gluten free food. Stopping the contamination also finally convinced my mother that I really did need to be gluten free, because she could see how much healthier I was without gluten.
I appreciate, more than I can say, all the hard work you do to make eating, and living, easier for all of us who NEED to eat gluten free. Your tips and explanations for finding ingredients, cross contamination, restaurant dining, and so much more are making this transition much less daunting and frightening.
Shirley Braden says
Hi Rebecca–It looks like this is your first comment on gfe–welcome! And thank you so very much for sharing your experience with us and leaving such kind feedback on my work at gfe. I truly appreciate it!
I don’t wish the gluten challenge on anyone and I can count on one hand the number of folks I personally know of who have tested positive for celiac after a gluten challenge and that number is a very small percentage of those I know of who have done a gluten challenge. As you say, it’s a horrific experience and not at all recommended because of what one must endure as far as symptoms, but it also can trigger other health conditions, including even other autoimmune conditions. The celiac testing of today requires total villous atrophy for one to get a positive diagnosis and because our bodies start miraculously healing to some degree once we go gluten free, a gluten challenge rarely yields positive celiac testing results. Most folks get a negative or “inconclusive.” So all that angst and bodily harm for naught. 🙁
All that said, I am so glad that you are gluten free again and totally on the right track, Rebecca! Figuring out the cross contamination factor is huge. I’m not glad that you kept experiencing the health issues after thinking you were being gluten free, but I am glad that both you and your mom saw it first hand, so you can take it seriously from this point forward. There are still long-time gluten-free folks who don’t take the cross-contamination concerns seriously, so they get glutened on an ongoing basis. Sadly, they’re part of the group that says they did not get better after going gluten free. 🙁
I am so very happy that I’ve been able to help you in transitioning to living gfe. It is overwhelming at first (and still on occasion it’s frustrating and overwhelming for me over 12 years in—that is reality), but it sure helps to have knowledge and strategies. Knowledge IS power for sure.
Best of luck and the best of health to you, Rebecca! Thanks so much for being a gfe reader and for taking the time to comment today!
Shirley
Cheryl DiBiase says
What a refreshing article. Thank you. I have been saying this for a long time.
I am biopsy diagnosed. I don’t WEAR that as some sort of badge. The medical profession failed me miserably. I was very close to death when I finally found a doctor who LOOKED at me. My labs were so bad that liver and kidney function showed ZERO in blood work.
The biopsy can reach ½ of 1% of the villi. That is less than 99% of the villi that are in reach. Of that they take 4 to 6 biopsies. That is less than ½ of a percent of the area they can reach that gets biopsied. No other deadly illness is treated with such pitiful testing methodology.
On top of this, they know very little about how the immune system works. The villi are just the one thing being damaged that is easily provable. I had horrific nerve damage. I get Central Nervous System symptoms as a first sign of being glutened. That happens far too fast to be due to villi damage.
Positive response to the gluten free diet should be a major factor in diagnosis. A profession with a decent amount of humility would face the fact that the human body is infinitely complex. People don’t choose gluten free without some good reasons. (I know we have fadders out there. Let’s ignore them for the moment.) It is hard to stick to gluten free. It is past time that patients be treated as CLIENTs with brains and partners in their healthcare.