Today I have the privilege of sharing another personal gluten-free story, The Beer That Saved My Belly. If you’ve been reading gfe for a while, you know that I am passionate about sharing personal gluten-free stories. Stories of diagnosis and recovery. It’s often when individuals hear personal stories of celiac or non-celiac gluten sensitivity that it “clicks” that they, too, have the same issues.
We can diligently read a listing of symptoms and perhaps nod our head a time or two, but we can also be quick to dismiss the possibility if we don’t have all of the symptoms listed. And most of us who are gluten free (after suffering from symptoms of gluten issues for years) know that gluten affects everyone differently. There is truly no “One Size Fits All” when it comes to how gluten affects us, so it helps to hear many stories to recognize that we may, in fact, have celiac or non-celiac gluten sensitivity.
The story I’m sharing today is that of Dr. Delise Dickard. Delise is a long-time friend and also a member of my support group. In a relatively short amount of time, Delise has become a relentless advocate for awareness on celiac/non-celiac gluten issues.
She recently participated in the Gluten-Free Labeling Summit in Washington, D.C., and met Dr. Alessio Fasano, director of the Center for Celiac Research and Treatment (now housed at MassGeneral Hospital for Children), in person there. Delise had previously interviewed Dr. Fasano as part of an excellent article she wrote on gluten sensitivity for our local newspaper prior to the Summit.
I applaud Delise for all her efforts and think you’ll very much appreciate her story. You can read a little more about Delise in her bio before her story.
Dr. Delise B. Dickard, is a psychotherapist in private practice at Camellia Cottage, which she founded. She previously founded and directed Riverside Counseling. In addition to her doctoral degree in Counseling Psychology, she has earned a Masters Degree from Harvard University in dramatic arts and is an award-winning playwright. She was also the mental health columnist for our local paper, The Free Lance Star, where her writing included the perils and delights of learning to live gluten free.
My story of gluten sensitivity likely began in my twenties with gastrointestinal symptoms. Doctors chalked it up to stress for a while but eventually gave me my first official diagnosis—IBS. It was oddly comforting to have some label to cling to and my form of IBS was politely called “D type”. “D” for Diarrhea.
As anyone with “D” type knows the problem is anything but polite, in fact, it is very disrespectful and can strike at the most inconvenient times. So I learned how to scope out the locations of restrooms much like people notice the exit doors upon settling in on an airplane. I also collected an arsenal of medications intended to save me from embarrassment when I was in various states of gastrointestinal distress.
I tried not to let it stop me from anything and, at age 25, took a four-month backpacking trip to Europe. Just to be digestively “safe” I stuck to a simple diet of wine (don’t drink the water!), cheese, and bread. I laugh to think I missed the entire culinary experience of Europe and clung to bread – my worst choice.
I have a memory of being so sick in Bulgaria that I couldn’t get out of bed. I was staying with a lovely family, but I was practically comatose. Had my own mother been there she would have naively fed me chicken noodle soup and saltines, but this mother came to my bedside with two huge bowls of food—one brimming with strawberries and the other filled with steamy boiled potatoes.

Fresh Glorious Strawberries (grown by and photo taken by Jennifer Smith)
The last thing I wanted to do was to eat and this wasn’t on my “safe” list. The berries were washed in Bulgarian water—OMG! I ate it anyway and I’ll never forget how utterly delicious this pure food tasted. I always said, “That food healed me!” It was the best meal I had in all of Europe—maybe ever!
I recovered and I was able to go on with my trip. I had a marvelous time despite the fact that upon my return I could have written A Traveler’s Guide to the Toilets of Europe.
By my thirties, I began developing what looked like rosacea. I had struggled with acne and rashes so this was no surprise. I just added heavy makeup to my growing bag of necessities.
Somewhere around 40, I began to notice white patches on my skin and was diagnosed with vitiligo, an autoimmune disease fondly called the “Michael Jackson” disease, so I added more makeup to my bag. Then Reynaud’s Syndrome was discovered, so just another autoimmune disease had emerged.
I could still function at a pretty high level and got various graduate degrees and opened my private counseling practice in Fredericksburg. Then my mid-forties brought on a list of symptoms that caused doctors to look at my age (then 45) and say “perimenopause.”
By the summer of 2010, I had become extremely sick. My biggest symptom (pun intended) was bloating. I had had cyclical bloating with my menstrual periods so everyone thought (again with my age now approaching 50) I was simply going into menopause.
I remember thinking: “If menopause is THIS bad then the entire population of women rounding 50 would be at home in bed!” But for two months I stayed bloated all of the time and felt so bad I could hardly function.
I felt like the doctors were just blowing me off. I needed to show how severe the bloating had become. I went to the emergency room twice and each time they immediately gave me a pregnancy test because I just looked pregnant. I even had one nurse pull me aside and smile knowingly as she said, “You know honey this can happen even at 48 … even with your husband’s vasectomy…” After the negative pregnancy test, I didn’t see HER again.
I had to buy clothes two sizes bigger thinking this was my “new normal.” I tried to hide my stomach. But I finally decided I needed to show the extent of the bloating to my doctors. I took two pictures one day apart. In one I was 41 inches and in the other, I was 36. When I showed them what would happen in the course of three hours this did get attention. One surgeon simply said, “Wow, that’s impressive.”
So I hauled around my pictures in a huge medical file labeled “What is wrong with me?” I went to five specialists. I got all those horrific tests where you drink gallons of stuff. They stuffed cameras into all sorts of places cameras shouldn’t be. I had exploratory laparoscopic surgery and hoped that the surgeon would find something that was wrong that could be fixed. He actually apologized to me when he told me I looked perfectly normal on the inside.
So I began to chart things: inches, diet, my cycle. The bloating seemed to come in random waves with pain so severe I couldn’t function. I actually thought I might lose everything—my family, my friends, my practice. But I just couldn’t accept this was my “new normal.” I had to know what was debilitating me. The specialists each gave a different final answer: hormones, chronic IBS, adenomyosis (don’t bother looking it up). The only proposed solution was a hysterectomy.
Just as I was ready to let them remove my perfectly normal uterus, I had an important day. I was feeling better. I went to lunch with my husband and had one frothy dark beer. It was, frankly, delicious. It was rare for me to have a beer for lunch and this one must have been loaded with gluten because in two hours I was swollen beyond belief.
I call it “The Beer that Saved My Belly” because after this beer my body “spoke” to the tune of about 7 inches of swelling. Thank goodness, I had a dinner date with my girlfriends. I remember dragging myself off the couch—refusing to let my huge belly pain interfere with my friendship.
So after all the specialists, various scopes, surgeries, and ER visits, I walked into the room with my girlfriends—tummy poking out of my coat. While one said,
“Oh my God, you look six months pregnant,” the other said, “You have gluten intolerance!”
Well, thank heaven for girlfriends! That was it—I had my answer.
I went on the diet that night and I was very very strict. I lost one inch per day in my waist. I felt significantly better in about five days. But I continued to lose inches (not weight) until I lost a total of 9 inches in two weeks without exercise, calorie counting, or any weight loss.
So my “new, completely unglutened normal” stomach measurement is about 32 inches. Unbelievable. I felt like someone from one of those crazy ads-–”drop two dress sizes in two weeks!”
Of course, I tested if gluten was really my issue a couple of times with reliable bloating results. I also tested positive by the Enterolab stool test. I also learned that I should have had a celiac blood test before going gluten free, because now I may never know where I am on the spectrum of gluten-related conditions.
I have learned that I am extremely sensitive and still get accidentally “glutened” quite often. I’ll know because three hours later all my uncomfortable symptoms return for a week. But still, I have not had an “intentional” crumb of gluten for over six months now. My body is healing and here is my list of improvements so far:
- I feel great.
- I’m back in clothes I wore five years ago.
- My rosacea has cleared.
- Various rashes are gone and, most astonishingly, the white spots of vitiligo are repigmenting. I’m wearing skirts again!
As challenging as it is for me to keep from getting contaminated, I am thrilled to finally KNOW I am gluten sensitive. I don’t see it as a disease. I see my gluten sensitivity as the information I desperately needed to learn about my body. I’ve thrown out my IBS meds along with my heavy makeup bag.
Living gluten free has brought so much health and well-being back into my life. Who would have known that as I round the age of 50 that I would look and feel better than I have in many many years! In fact, now that I feel good again, I think I’m going to need another trip back to Europe. I hear they have really good strawberries and potatoes!
Shirley here:
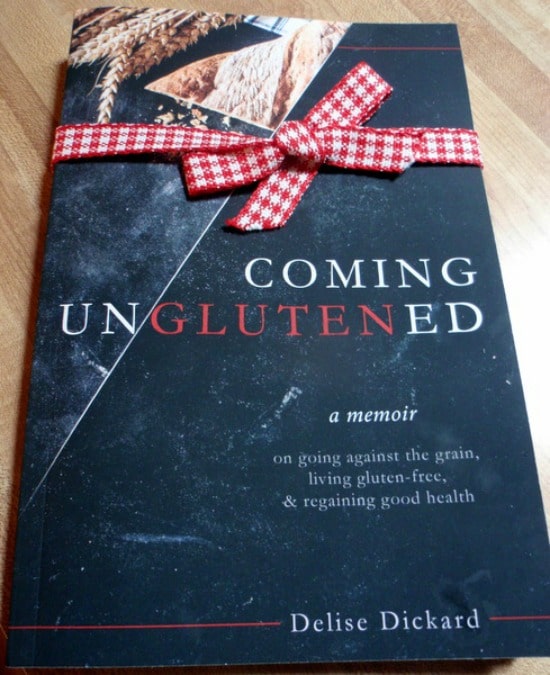
Since this post, Delise has published a book sharing her complete story, Coming UnGlutened, which goes way beyond her personal gluten-free story: The Beer That Saved My Belly. You can read my review on gfe here. Spoiler alert: It’s most definitely worth a read!
Here are some other very compelling personal gluten-free stories that have been shared on gfe:
- From Ginny Ryan: “You’re Not Crazy, You’re Sick, and You May Have Celiac”
- From Ginny Ryan: “In Defense of the Medically Necessary Gluten-Free Diet”
- From Linda Etherton (Gluten-Free Homemaker): “My Personal Celiac Story”
- From Debi Smith (Hunter’s Lyonesse): “My Journey to Healthy Living”
- From Diane Eblin (The WHOLE Gang): “I Can’t Eat What and It’s Where?”
- From Dana (Home*School*Home): “My New Gluten-Free Life”
- From Cheryl Harris (Harris Whole Health and Gluten-Free Goodness): “The Role of Food in Inflammation”
Last, here’s my guest post on celiac and non-celiac gluten issues over at Anali’s First Amendment.
Originally published May 19, 2011; updated December 8, 2021.

glutenfreeforgood says
Great post Shirley and Delise! I can relate to this one for a variety of reasons. First off, I love Dr. Fasano. As you know, Shirley, he was my doctor. He’s wonderful (and very cute).
Delise, your symptoms and story sound so much like my daughter’s. She went to college in London and consumed a diet of bread, fish and chips. She was always sick. She had vitiligo, intestinal issues, alopecia, eczema, rashes, migranes, etc.
It’s such a shame that it’s so difficult to get a diagnosis! I’m glad you’re on the path to increase awareness. I’m passionate about that as well (as is Shirley).
By the time my daughter got her master’s degree at the U of Glasgow in Scotland, we had figured out her problem. She did fine in Scotland and was even able to get gluten-free Kit Kats, which she was thrilled about. =)
Bottom line though — you’re right, whole foods (strawberries and potatoes are perfect) are the answer. No “ingredients” and no labels to read!
Melissa
Delise Dickard says
Isn’t is crazy that our Doctors aren’t advocates (or even aware of this simple, healthy, answer. Thanks for he comment and good luck to you. Delise
Lauren @ As Good As Gluten says
What a great story, thanks for sharing!
cheryl says
Thanks so much for sharing your story and your passion, Delise! (and thanks, Shirley, for sharing Delise with us)
Ditto on Dr. Fasano, Melissa!! I figure if I’m going to spend a Saturday hearing about villus atrophy, I’d prefer it be from someone with a delicious Italian accent.
Delise Dickard says
NO kidding about the accent! And the doctors do respect him when I quote him. Take care, Delise
Debi says
Delise, thank you for sharing your story! It’s so inspiring to see another person who found gluten to be their nemesis after so many tests and diagnoses. I’m glad you finally found your answer and are seeing good results. 🙂
Delise Dickard says
Yes, I just have to lose my hope of finding more than one doctor who will believe this is the culprit. So far that’s a challenge. Delise
Nancy @SensitivePantry says
This story is probably the story of so many people who have yet to be diagnosed with gluten intolerance or celiac disease. Thanks to Delise for sharing and Shirley for hosting–I hope many people come here, read this, and decide to push their physicians for a definitive answer. Or, if that fails, just simply remove the gluten from their lives.
So happy, Delise, that you have found good health and new energy. When people ask me if it’s hard to be GF I look at them and ask what the alternative is–leading a sickly life? No, it’s not hard at all!
Maggi says
Delise – thank you so much for sharing your story. And in so many ways, it is exactly the same as my story. It’s really sad that as a medical professional, you weren’t lent any more credence to your condition than the average person. But I suppose that’s not too surprising. What is surprising is why is this happening to so many people and numbers keep rising?
InTolerantChef says
Great to hear your story of restoration. It’s amazing that so many horrible symptoms are so hard to diagnose. You have to hope that the medical profession starts to go to gluten intolerance sooner rather than later!
Delise Dickard says
To all,
How validating to read these comments. It truly brings tears to my eyes. When I think about how lonely it would feel without the the internet and Shirley’s wonderful site, so many of us would feel alone..maybe even a bit crazy! I know I would.
I’m not a medical doctor, I have my doctorate in Psychology. Still it is unbelievable how many times I’ve heard: “Well you know stress…” or “Sometimes if you believe something,it becomes true…”
I do have two ideas for dealing with skeptical doctors. One Doc told me “We are scentists, so we need to see scientific evidence.” So, I’ve started bringing a big pile of scientific journal articles with me. I’ll post my favorites later today. They’ll know you are no dummy and they are relieved if you just give them one to read.
Second, Dr. Fasano told me, with regard to gluten sensitiity, you must rule out everything else. It wasn’t what I expected to hear but it does make sense. So when skeptical doctors test for other things (within reason), I now think it is probably a good idea — just in case.
He also said that celiac disease should definately be on the list — at the top, in the middle, or the bottom. It is simple enough to get the Ttg blood test, but of course you have to do it before going gluten free. If it were up to me I’d make the test manditory. In all those months they gave me half a dozen pregnancy tests (I’m 49) but never the Ttg for celiac. Now I’m gluten free and I’ll never know about celiac.
Thanks again for all the comments. Its a gift to have found this community.
Delise
Heidi @adventuresofaglutenfreemom.com says
Delise,
Your story gave me goosebumps, thank you so much for sharing it! No doubt you will help many people who are struggling with similar symptoms. I am so utterly fascinated by how gluten can effect people so differently. I myself, am asymptomatic for gastrointestinal symptoms. Gluten largely attacked my skin (eczema, psoraisis, dermatitis herpetifomis) and my brain (depression, ADHD, and severe mood swings) and that is why I lived somewhere on the spectrum of gluten sensitivity for nearly 30 years before I was finally diagnosed with celiac (and now I have a total of 5 autoimmune disorders!).
Your saga with bloating sounds so much like what my uncle had for many years. Of course, they couldn’t run a pregnancy test on him, so his Dr. just diagnosed him with “tight belt syndrome” and told him to loosen his pants after he ate. Sadly, he would pass away from non-Hodgkin’s lymphoma (a cancer that celiacs are at great risk of developing) several years later.
You may not know officially where you fall on the spectrum, but in the end, the treatment is the same and so is the wonderful gluten-free community that surrounds us. I am so happy that you found your answer…and I have heard that European strawberries are absolutely divine! 😀
Hugs,
Heidi
Delise Dickard says
Heidi,
Your response is so interesting. My father actually has the same symptoms as you only he says “I have no symptoms” because he has no bloating or intestinal upset. His mood swings are extreme (bipolar disorder) and the rash comes every summer on his hands. My mother went gluten free when I did and just felt so much better she’s never gone back. My father (because she’s the main cook) went gluten free by default. They went on vacation and the moment he went back to gluten he got sick, really sick. He kept eating it and ended up in the hospital for several days. He went off gluten, recovered, then got sick again the first time he had a handful of croutons. The upshot is he’s still off of gluten because he’s scared to eat it but won’t admit intolerance. The most unbelievable part is that, despite my pleas, no doctor will give him a celiac blood test. Soon he will have been off of gluten so long (maybe already too long) it will be too late for an accurate test. Thanks for your kind response. We obviously share some genetic links. We also have a number of autoimmune diseases in the family. I wish you good health. It sounds like you are on the right track. Delise
Jennifer Preston says
I can relate to this story SO well. I had Fibro, bloating, terrible rosacea, and some unmentionables. I also had a full hysterectomy and then went GF bc my young son was allergic to wheat. A huge relief of chronic symptoms in my life was relieved and I have no doc to give me proof. Just an awesome life of moving on and enjoying the life I saw others having. Thought I was dying at one pt….now feel ‘normal’. Thank God for this community….others don’t get it at all.
Carol, Simply...Gluten-free says
Great post Shirley. Thanks for sharing these personal stories, it is so helpful to others. I agree with Jennifer, thank God for this community and for you – your passion and dedication to this community is tireless!
xo,
c
Sarena (The Non-Dairy Queen) says
Thank you for sharing this story! It makes me think of Tony. He suffered for years and was told he had GERD. He had horrible bloating, migraines, numbness in his fingers, arthritis pain, extreme fatigue and he was gray. It was horrible to watch. It’s stories like this that help others realize what they are going through and how to help themselves. Thanks again for sharing!
xo
Sarena
Delise Dickard says
It so sad to hear of such suffering, and what just ties me up in knots is that the medical community should know to look for this. Even if they don’t fully believe it, it doesn’t hurt for them to have it on a list of possibilities. It is stories like yours, Sarena, that make me want to drop everything and promote awareness among the medical community. My hope is that, now that more solid scientific evidence is being published, we can get these studies into the hands of the doctors quickly. But its communities like Shirley’s that give me strength and motiviation –otherwise I would feel very much alone. So thank you for sharing. Delise
Shirley says
Thanks so much to you, Delise, for sharing your personal story. Obviously it resonates with many who have commented here and I’m sure just as many (or more) who are reading it without leaving a comment. We truly don’t know the full impact these stories can have. Sometimes they just plant a seed in a reader’s mind that may eventually lead to a celiac/gluten intolerance diagnosis and healing through the gluten-free diet. That’s huge! Thanks so much to the rest of you who took the time to comment. I really appreciate you sharing your stories and giving Delise feedback and support!
Hugs to all,
Shirley
Alta says
Delise, this is a great story and one that I certainly hope can help many others struggling with these kinds of issues and thinking it’s just “part of life” or “part of getting older”. Bloating like you described was one of my major symptoms too – and no, it’s not something you have to live with! I can imagine you’re so happy to feel better.
Ashen says
I was wondering if anyone here has been diagnosed as having foliculitis (it’s a really itchy rash) My Dr. treated it with antibiotics for 10 days, but I still have it. The more I’ve been reading the more I am thinking it might be DH.
I am definitely asking my Dr. to do a gluten test. So many of the symptoms posted for gluten problems sound like what I’ve been dealing with.
Thanks for any help anyone can give me.
Shirley says
Hi Ashen–Welcome to gfe. Since this post was published a while ago, I’m not sure that enough people would be reading it still to expect any answers from others. It could be likely that either you’ve been misdiagnosed or that you do actually have folliculitis, but that it’s related to gluten. Son was diagnosed with folliculitis a few times as well as other skin conditions, but all went away when he went gluten free. The dermatologist did not do the biopsy for DH correctly. It can’t be done on the lesion itself. It has to be done a certain distance away from the lesion, but I didn’t know that then. Also, folks who have DH may not have intestinal damage so those individuals will not test positive for celiac via an endoscopy. But a DH diagnosis means celiac disease.
Here are two links below that I found on folluculitis. Note that these are forum comments, not medical articles. I am sharing them because some mention gluten and some mention treatment ideas that seem reasonable.
http://www.celiac.com/gluten-free/topic/80812-persistant-folliculitis/
http://www.topix.com/forum/drug/accutane/T2FDG18EB0H86D2MD/p3
Numerous skin conditions can be caused by celiac/gluten intolerance or non-celiac gluten sensitivity. As Dr. Rodney Ford says, gluten affects gut, brain, and skin. He also talks about it here in one of his YouTube Videos. He’s a “character” of sorts, but a wonderful one, who is so well versed in this area.
I hope you get proper celiac testing done. However, if that’s negative, please follow up with testing for non-celiac gluten sensitivity. Finally, some folks decide to just go on a gluten-free diet, but I think getting some type of validation can keep one committed to a strictly gluten-free diet. Best of luck, Ashen. Feel free to write later. I’m happy to help if you go gluten free and need pointers. And I will share this on my Facebook page and see if anyone else has any particular experience with folliculitis.
Shirley
Kerry P says
I suffered for years with what I called “infected hairs” on both my scalp on body. It was like a whitehead, with a hair growing out of it. It wasn’t until after I’d been G/F for several months, that I realized the problem had been corrected.
Delise Dickard says
I had so many random problems go away, I don’t think anyone knows all the ones that are related. You just get healthier in so many ways. Delise
Delise Dickard says
I had an interesting addition to my story. I’ve been in search of one gastrointerologist who repects my gluten intolerance. I went to one who insisted on an upper endoscopy to “prove” it was celiac. An extensive biopsy showed no villa atrophy whatsoever. I went to another, showed him the results and said I simply wanted one gastrointerologist who respected my gluten intolerance. This one said “Well it has not been scientifically verified, you may not be intolerant.”
“Just give me a cracker” I’m thinking but he gave me a blood test for the celiac genetic markers and guess what? No celiac markers. So he called to gloat and my husband answered. When he told my husband I was NOT intolerant my husband refered him to the Jan. study out of australia showing that the celiac markers were not accurate for gluten intolerance without celiac. The upshot — I still can’t eat a cracker without reliable results (after 3 hours bloating, sometimes gastro trouble and always a red face for a week). Unfortunately we can’t rely on the Doctors yet…I’m still hoping. Delise
Ashen says
I am going to give my Doctor a chance. If i get a positive diagnosis I will at least know i am right. I am pretty sure this rash is either not folliculitis or is in addition to it. I have blisters where there are no hair follicles.
Yesterday afternoon (before I read any of this information about gluten intolerance) I had a cookie. Within a few minutes I had indigestion. After an hour the itching I have been experiencing increased (pre-cookie the itching was almost gone). Right now I am certain there is something in that cookie I should not be eating. I will wait for testing, because there may be more than one food I have problems with.
Thanks for all the comments. It’s nice to know I am not going clinically nuts from all the itching. It just feels like I am.
Delise Dickard says
From my discussion with Dr. Fasano I learned that he would probably say you are doing the right thing. He said to let the doctors rule out anything that can be verified clinically. (I would add be careful about letting them remove organs as they almost removed my uterus.) But once everything else is excluded (including celiac) you can try to figure out if gluten is the culpret. I hope you get relief soon. Delise
Ashen says
Update: I went to the doctor yesterday. It turns out I have type 2 diabetes. It might have been the sugar in the cookie i was reacting to. I have some appointments scheduled for a nutritionist. I will work with him/her to find out if there is a gluten problem. I don’t want to try it without that help, because diabetes is scary stuff. I am not going to do anything that can cause me to have more problems. I already know that I am so allergic to nickle that i can’t eat canned food, or have any surgery where they use stainless steel implements. My daughter was a c-section, and I had severe blisters in every spot where they used clamps. If they want to remove something they have to prove to me that it will save my life and that there is no other way.
Shirley says
Hi Ashen–I’m so glad you are finding more answers. I’m very sorry about the diabetes diagnosis, but it sounds like you are proactive and will do all you can to be healthy. Folks can even reverse diabetes with proper diet. Just note that often standard diet guidance for diabetes can fall short. I’m reading the book Sugar Nation right now, which is a bit of an expose. It summarizes what I have learned before … that standard diabetic diet guidance focuses too much on carbs, and still inappropriately severely limits proteins and fats. Do your research and yes, get tested for celiac/non-celiac issues as soon as possible. Folks with Type 2 diabetes have a much higher incidence of celiac disease, and even without celiac disease, glucose and gluten issues are often related. The nickel allergy definitely complicates your life–wow. I’m not allergic to nickel, but I was allergic to the material that my dissolvable stitches were made of when I had surgery. They never dissolved and I did not fully heal (months later) until the stitches were extracted manually. I do think that many of us who have celiac/gluten issues tend to have a multitude of other issues that go with them. I’m truly so sorry you’ve been through so much, dear. Please keep pushing for proper celiac and non-celiac testing to make sure you’ll be going down the completely right path as you change your diet.
Hugs,
Shirley